Business need
It became evident that the Customer’s billing system that was in use since the 1980s lacked the necessary functionality and no longer was current with technology. The system was DOS-based and had not changed much since its initial development. As Customer’s employees grew accustomed to Windows programs, operating this system – that also inconsistently wrote checks and randomly froze up and shut down – became increasingly difficult. As a result, it was decided to replace the old automated system
Solution
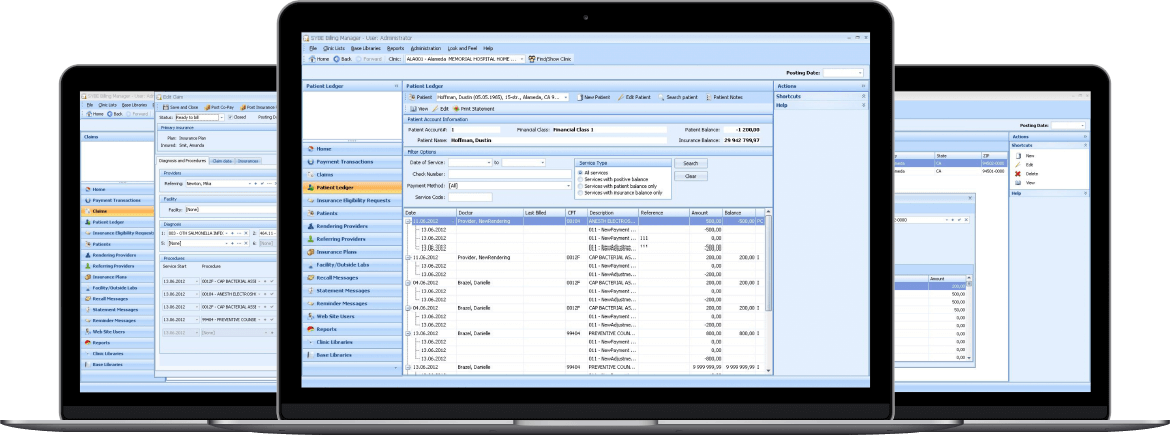
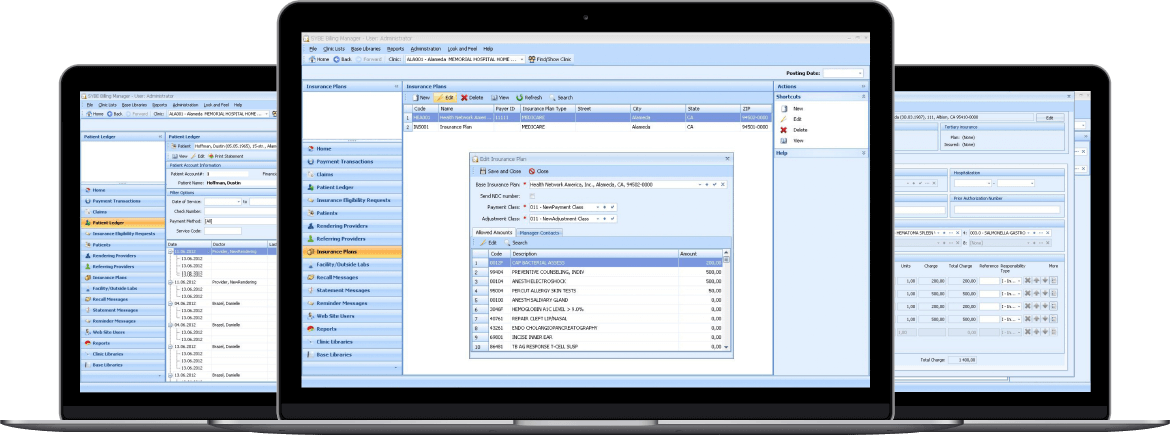
All efforts resulted in a new client-server medical billing software with multiple security layers and role-based access levels.
Our Customer is a well-known American medical billing organization with operations all over the USA. The company provides its clients efficient medical billing and credentialing services.
- To integrate the latest technology and industry standards into the new solution.
- To maintain high productivity levels after the new billing system’s implementation.
- To train the Customer’s team on using the new software.
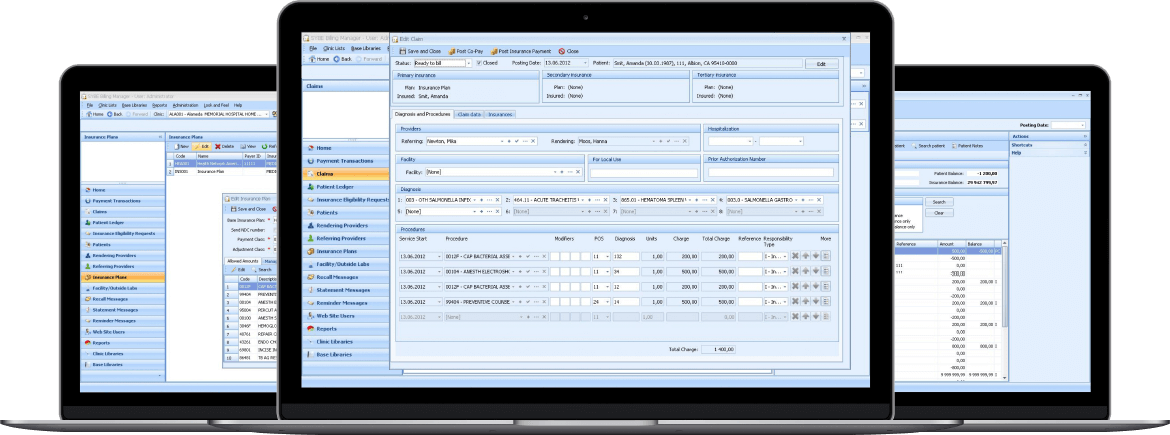
- To optimize the process of submitting and following up on CMS-1500 claims to insurance companies.
- To make the system compliant with HIPAA and HL7 regulations.
What was achieved:
- the implementation of the new solution allowed the Customer to improve its competitiveness, compliance and efficiency;
- the claims status and payments tracking ability resulted in a 30% increase in the number of clients;
- the productivity of each Customer’s employee increased by 27% through the reduction in time spent on each claim.
technologies
- WinForms
- DevExpress components
- ASP.NET Web Forms
- JavaScript
- NHibernate
- MS SQL Server
- WCF
- Windows OS
Project Results
As a result of this project, the new medical billing software optimized the process of submitting and following up on claims to insurance companies. All of the billing processes were required to go through a review, reengineering and documentation according to proposed functionality compliant with HIPAA, HL7 and ODB regulations. This effort included the planning of how to depict each control and process, developing the expected results, documentation of the process and control evidence. The medical billing software developed by Softarex Technologies, Inc. included the following features:
- User Authorization: only verified users were permitted to access the application;
- Role-based Access Levels: all users were divided into two groups with different access rights – Administrators and Managers;
- Multiple Security Layers: a set of privileges was defined for each user;
- Clinics/Doctors Information Management: the ability to create and manage all information related to healthcare providers using the system;
- Insurance Eligibility Verification: real-time updating and confirmation of patients’ insurance status;
- Tracking: the ability to check each claim’s status, payments and office workflow;
- Reporting: the opportunity to create comprehensive billing reports as well as custom claims reports;
- Services and Payments/Insurance Companies/Providers/Patients: the ability to create and manage all information required to fill out the CMS-1500 claims.
On top of the above functionality, the medical billing solution easily alleviated all reminder tasks: for any task or calendar event, it was possible to create a reminder and see a pop-up window with a notification message about the upcoming event. Besides, it became possible to send messages to patients from the billing company’s office to remind about the services that were rendered earlier and needed to be paid for. Moreover, easy and quick integration with a possible statement-mailing third-party service was stipulated and successfully implemented. The Customer’s employees admitted that one of the biggest benefits of having Softarex Technologies, Inc. as their system support provider was having “Technical Support people who can talk to ‘non-computer’ people and get the problem fixed”. The company also commented that the support staff was very prompt in returning calls and fixing problems.